Reading Time: 6 min.
They come in all shapes and sizes and have various routes of administration: Hospitals carry a wide range of medications. Storing them safely before administration to the patient while also remaining easily accessible to the nursing team can be really challenging. However, this challenge can be solved with automated dispensing cabinets (ADC). Besides safe storage and support for caregivers in providing accurate and secure drug dispensing at the clinical points of care, the digitized medication inventory makes mundane tasks like replenishment orders, expiry date controls and inventory counts obsolete. Adding an ADC to your point of care positively contributes to both patient safety and operational efficiency.
3 Benefits of ADCs
ADCs can securely store and dispense medications at various clinical points of care like wards, operating rooms, emergency rooms and even in intensive care units. The computer-based system connects with the hospital information system (HIS) and the computerized physician order entry (CPOE) to:
-
digitally record all drug-related transactions which enables full drug traceability,
- provide LED-light guidance to accurately pick and dispense the right drug for the right patient,
- enable quick onboarding for new caregivers.
The ADC reinforces a closed loop medication management from the hospital’s central pharmacy to its points of care for various drugs including narcotics, controlled substances and high-risk drugs.
Main benefits at a glance
- Improved medication management practices increase patient safety.
- Increased operational efficiency for both nursing and pharmacy staff.
- Improved drug inventory reduces medication waste and loss.
1. Improved medication management practices at points of care increase patient safety
Dispensing is visually guided and significantly increases patient safety because manual errors at the points of care are reduced: LEDs on the exterior of the drawer direct the caregiver to the right drawer; the drawers are mechanically unlocked.
Besides those measures, the requested medication is also graphically shown on screen. Further special configurations for the individual safety requirements of facilities are also possible:
- The storage compartment that contains the requested medication can be lit up to guide the caregiver to the right drug.
- Narcotics, controlled drugs, high-risk drugs and expensive drugs can be stored separately in one dedicated drawer to solely unlock the necessary compartment.
- Preset a second verification before a high-risk drug is dispensed from the sliding drawer for an extra layer of safety.
The second verification is available in different formats. The Clinical Data Messenger (CDM) of an ADC can either simply display a pop-up notification with a warning or request the user to put in extra information about the state of the patient such as blood pressure readings when Amlodipine is requested. Such warnings also mitigate the risk of confusion for look alike sound alike drugs (LASA): The CDM warns users with a confirmation alert to ensure the correct LASA medication is dispensed in the right dosage.
ADCs support the process of drug administration by reinforcing the 5 rights of medication. First, the medical staff selects the patient on the screen, next, they are guided to pick and dispense the correct medication in the right dosage as defined in the electronic patient prescription. Dispensing alerts for drugs that are dispensed too early, too late, or too close to a predefined administration timing are shown on-screen to notify caregivers during the dispensing process. All this ensures that the right drugs are administered at the right time in the right dose with the right route of administration.
2. Increased operational efficiency for both nursing and pharmacy staff
By digitizing all drug-related transaction records like dispensing, replenishment and drug returns, ADCs significantly improve drug management processes. On the basis of this digitization, replenishment orders for drugs below par levels are automatically sent from the ADC to the central pharmacy. Times of receiving multiple replenishment orders a day are a thing of the past.
Various compartments within the drawers of the ADC are set up for storage. As mentioned before, lights on the exterior as well as graphic on-screen guidance support correct dispensing processes. The replenishment process is similarly light-guided to ensure accurate loading. Furthermore, digital guidance based on the replenishment order list guarantees that the physical drugs which are sent from the central pharmacy tally with the order from the ADC.
Instead of time-consuming manual recordings for controlled drugs, inventory counts and reports on usage are available at the touch of a button. Intermittent counts of drugs make it possible to catch discrepancies early. Your current drug inventory can also be digitized and expanded by adding an ADC to your existing storage shelves.
Three login options, user-specific language settings and an intuitive design foster high usability and create fast and efficient workflows – even onboarding processes for new caregivers are smooth and easy.
3. Improved drug inventory at points of care reduces medication waste and loss
A patient’s condition progresses and the respective drug therapy changes accordingly. It often happens that pre-dispensed medications have to be disposed of due to adjustments in the prescriptions. An ADC that is connected to the hospital’s CPOE system is constantly updated with the latest prescription of each patient, avoiding that pre-dispensed medication is discharged because the drugs are not in the original package anymore and therefore not suitable for reuse.
In case dispensed medication is no longer needed because a therapy changed but the drugs are still in their original packaging, they can be returned to stock. This can either be the ADC stock or the internal return bin of the ADC. Authorized personnel can access and check that drugs of the bin are sent back to the central pharmacy for re-distribution. The return process for each drug is predefined in order to avoid hospital-wide overstocking of medication.
Internal pharmacy software of an ADC ensure full traceability and accountability of returned medication. It also manages expiration dates of the drugs stored in the clinical ADC network: On-screen alerts for impending expiring medication can be preset to reduce discarding of expired drugs.
Another inventory improvement is the possibility to extend storage capacities with an external lock for medical refrigerators. The integrated software displays an alert in case of temperature or humidity deviation to eliminate medication waste that is caused by improper storage conditions.
Summary: ADCs simplify the point-of-care drug management processes
Automated dispensing cabinets positively impact the medication management process at clinical points of care and strengthen the closed loop medication management. Accurate picking and dispensing processes increase patient safety; operational processes for caregivers on the wards and pharmacy staff at the central pharmacy become more efficient while medication waste is reduced.
Are you also affected by such challenges in your medication management workflow? Try out the ADC configurator to see which configuration meets your needs or arrange for an initial consultation with us today.
About the author Julian Vogelsanger
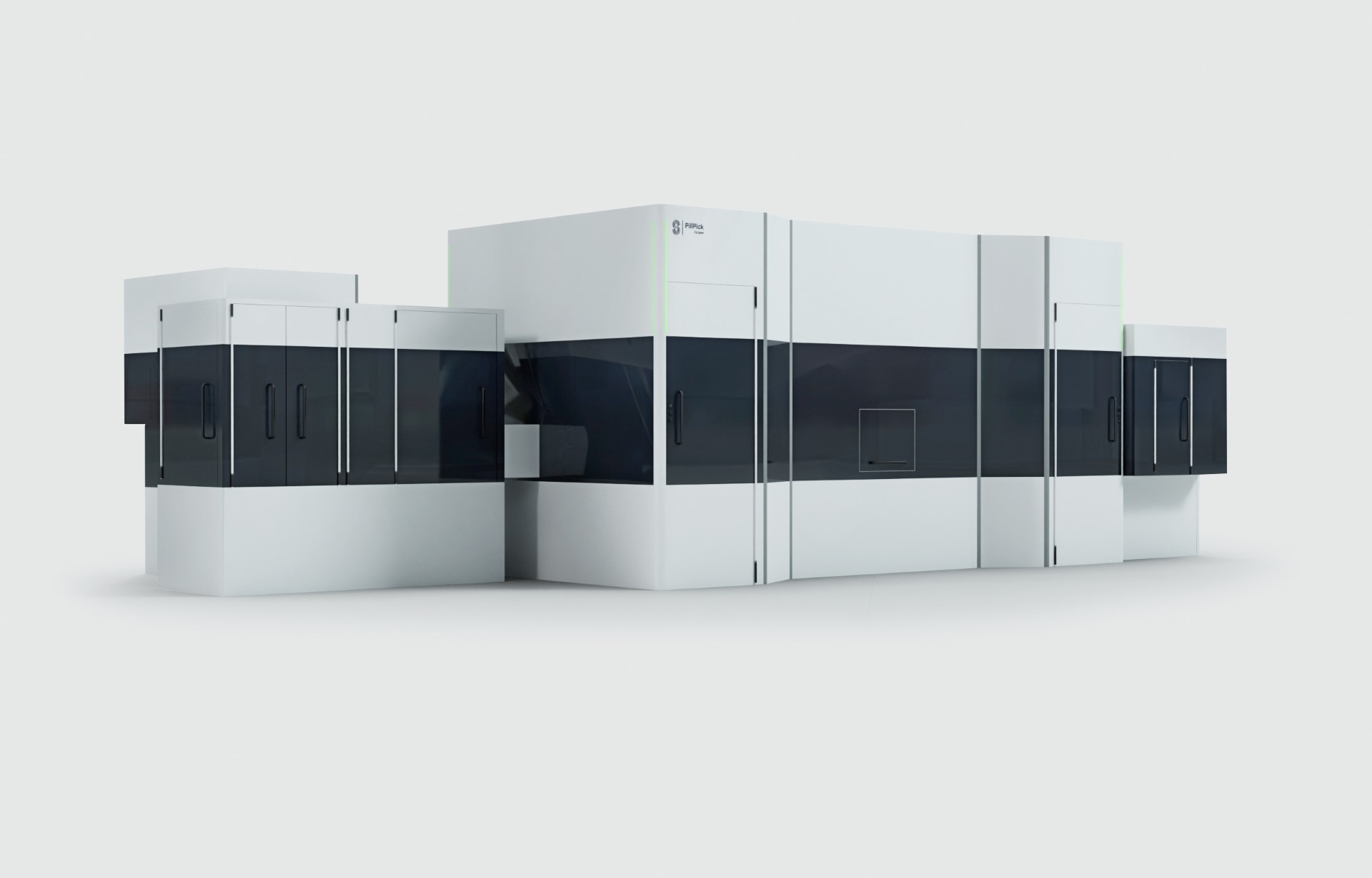
In his work in product management at Swisslog Healthcare, Julian relies on his strong technical background in mechanical engineering. His main focus is our PillPick and MedSMART, but he also works on broader product initiatives in transport automation and OEM products.